When and Why Do Parasomnias Occur During NREM vs. REM Sleep?
Parasomnias are unusual or undesirable physical events that occur during sleep. At Koala Center For Sleep & TMJ Disorders, our providers specialize in understanding these disruptive behaviors by pinpointing where they originate in the sleep cycle. The timing is crucial: different parasomnias are exclusively linked to either NREM (Non-Rapid Eye Movement) deep sleep or REM (Rapid Eye Movement) sleep, allowing us to diagnose the precise underlying mechanism. For more information, please contact us today or request an appointment online. We have convenient locations in Bloomington IL, Peoria/Dunlap IL, Mishawaka IN, El Paso TX, and Wausau WI.
Table of Contents:
Which primary sleep stage (NREM or REM) is associated with complex motor behaviors like sleepwalking (somnambulism)?
Is sleep paralysis a phenomenon related to falling into REM sleep (hypnagogic) or waking from REM sleep (hypnopompic)?
How does a sleep specialist use the stage of origin to accurately diagnose a specific parasomnia?
Does a sleep study (polysomnography) monitor for the presence of NREM vs. REM parasomnias?
The Koala Center Insight: Mapping Parasomnia Triggers to the Sleep Cycle
FAQ
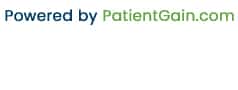
Understanding when parasomnias occur within the sleep cycle is one of the most important clues in determining their cause, severity, and appropriate treatment plan. Some parasomnias appear in the deepest stages of NREM sleep, while others arise from REM sleep—the stage where dreaming and temporary muscle paralysis happen. At Koala Center For Sleep & TMJ Disorders, mapping these patterns is central to diagnosing childhood and adult sleep disorders accurately. Knowing the sleep stage of origin helps distinguish between normal sleep behaviors, benign parasomnias, and more complex conditions that require medical attention.
Complex motor behaviors—such as sleepwalking, sleep terrors, confusional arousals, and sleep-related eating—almost always originate from deep NREM sleep, specifically N3, also known as slow-wave sleep. This is the stage when the brain is least responsive to external stimuli but the body is physically capable of movement. Because consciousness is only partially “offline,” the brain can generate behaviors without full awareness or memory of the event.
Children are particularly prone to NREM parasomnias because they have a higher percentage of deep sleep and immature arousal systems. During transitions in and out of N3, the brain may trigger movement while cognitive regions remain disconnected. This is why kids who sleepwalk often appear confused, do not respond logically, and have no recollection of the episode afterward.
Sleepwalking rarely comes from REM sleep because the body is normally paralyzed during REM—a built-in neurological mechanism that prevents us from acting out our dreams. When REM paralysis fails, it usually indicates an entirely different disorder known as REM Sleep Behavior Disorder (RBD), which is uncommon in children and typically seen in older adults.
Sleep paralysis is closely tied to REM sleep and can occur during two transitional moments:
● Hypnagogic sleep paralysis: When falling asleep
● Hypnopompic sleep paralysis: When waking from sleep
In both cases, the brain remains partially in REM mode while consciousness returns more quickly than muscle control. Because REM sleep involves physiological paralysis, individuals become aware of their surroundings but cannot move or speak. This mismatch between brain and body can feel frightening, and some people experience hallucinations because dream imagery overlaps with wakefulness.
Unlike NREM parasomnias, sleep paralysis is not associated with walking, talking, or motor activities. Instead, it reflects a temporary timing error in the shutdown and reactivation of REM atonia. A sleep specialist will view this as a REM-related parasomnia rather than an arousal disorder.
The sleep stage where a parasomnia begins helps clinicians determine whether the behavior is benign, developmental, associated with stress, or related to a more complex neurological or airway problem. For example:
● NREM parasomnias—such as sleepwalking or night terrors—suggest incomplete arousal from deep sleep. These typically occur in the first third of the night, when N3 sleep peaks.
● REM parasomnias—such as nightmares, REM Sleep Behavior Disorder, or sleep paralysis—occur in the latter half of the night, when REM cycles become longer and more frequent.
This timing gives a sleep specialist key diagnostic clues. If a parent reports violent movements during the early night hours, it points toward an NREM arousal disorder. If the events occur closer to morning with dream enactment, vocalizations, or purposeful limb movements, REM-related parasomnias become more likely.
Beyond timing, the stage of origin can reveal whether other medical issues are involved. For instance, fragmented or unstable sleep from obstructive sleep apnea may trigger repeated NREM parasomnias. Conversely, medications affecting REM sleep can increase REM-related disruptions. Identifying the stage helps pinpoint the root mechanism rather than treating symptoms alone.
A polysomnography (PSG)—a comprehensive overnight sleep study—monitors the architecture of sleep, including transitions between NREM and REM cycles. This allows our specialists to correlate abnormal behaviors with precise sleep stages. During the study, sensors monitor:
● Brain waves (EEG)
● Eye movements (EOG)
● Muscle tone (EMG)
● Breathing patterns
● Heart rate
● Leg movement
● Video and audio recordings
The combination of EEG and EMG signals is particularly important in determining whether paralysis is active (indicating REM) or if the patient is in slow-wave sleep (indicating NREM). Video monitoring provides additional insight, allowing clinicians to analyze behaviors as they occur—something parents rarely get a clear view of at home.
Tracking parasomnias in this controlled environment is vital for diagnosing conditions such as nocturnal seizures, REM Sleep Behavior Disorder, or apnea-triggered arousals. Each of these originates from different sleep stages and requires very different treatment approaches.
At Koala Center For Sleep & TMJ Disorders, understanding why parasomnias occur is just as important as identifying when they occur. The KoalaKIDZzz® model emphasizes a full-cycle evaluation of each child’s or adult’s sleep architecture. This includes assessing sleep quantity, environmental triggers, airway function, neurological patterns, stress levels, and behavior during transitions between sleep stages.
Our specialists use a “sleep cycle mapping” approach, which allows us to:
● Determine which stage consistently produces parasomnia episodes
● Identify triggering factors such as sleep deprivation, anxiety, or airway obstruction
● Analyze whether the parasomnia is developmental, medical, or neurological
● Build a tailored treatment plan targeting the specific stage of disruption
By connecting triggers to the exact phase of the sleep cycle, Koala Center For Sleep & TMJ Disorders can provide families with strategies that reduce episode frequency and improve overall sleep stability. This method ensures treatment is precise, targeted, and grounded in the unique physiology of each patient.
1. Are NREM parasomnias dangerous?
They are usually benign but can become risky if a child leaves the bed or wanders, so safety planning is important.
2. Do REM parasomnias always involve dream enactment?
Not always. Some REM disorders involve paralysis or vivid nightmares without physical movement.
3. Can both NREM and REM parasomnias occur in the same patient?
Yes. Some individuals experience mixed parasomnia patterns, which is why expert evaluation is essential.

Additional Services You May Need
▸ KoalaKIDZzz®
▸ Sleep Apnea
▸ Snoring
▸ TMJ Disorder
▸ Fatigue
▸ Sleep Disorders
▸ Weight Loss
▸ CPAP Alternative
▸ Oral Appliances