Is My Insomnia Secretly Causing My Chronic Migraines?
The link between insomnia (the inability to fall or stay asleep) and chronic migraines is well-established, creating a damaging cycle of pain and rest deprivation. At Koala Center For Sleep & TMJ Disorders, our providers specialize in diagnosing this connection by exploring the underlying mechanisms—such as fragmented REM sleep and increased nervous system excitability—that turn poor sleep into severe headache pain. For more information, please contact us today or request an appointment online. We have convenient locations in Bloomington IL, Peoria/Dunlap IL, Mishawaka IN, El Paso TX, and Wausau WI.
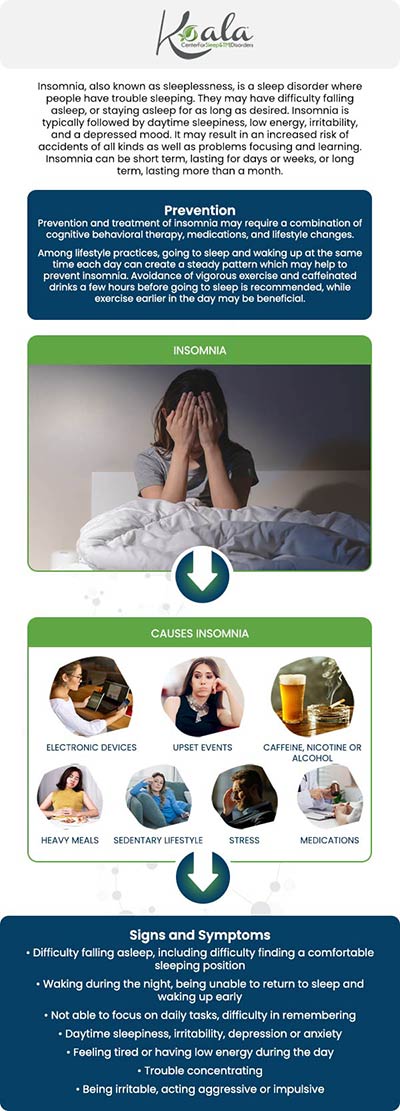
Table of Contents:
Can insomnia actually trigger chronic migraines?
How does poor sleep affect the brain and contribute to migraine attacks?
Is there a difference between occasional insomnia and sleep deprivation that leads to migraines?
When is it time to consider a full sleep study for chronic migraines?
El Paso Migraine Relief: Getting the Rest That Stops the Pain
Quick FAQ
Many people treat migraines and insomnia as two completely separate problems, but for countless patients, they are deeply connected. Poor sleep can make migraines more intense, more frequent, and harder to treat, while chronic migraines can make sleep fragmented and unrestful. If you wake up with headaches, notice migraines developing after sleepless nights, or feel like your brain never fully rests, insomnia may be the hidden trigger behind chronic migraine episodes.
At Koala Center for Sleep & TMJ Disorders, we help patients understand how disrupted sleep affects the brain and why correcting insomnia can dramatically reduce the frequency and severity of migraines—sometimes more effectively than medication alone.
Yes. Insomnia can directly trigger migraines, and in many patients, it becomes a primary factor in the development of chronic migraine patterns. When your brain does not receive restorative sleep, the pain-processing regions become hypersensitive. This means normal stimuli—light, sound, movement, stress, or hormonal shifts—can more easily activate a migraine attack.
People often believe migraines “just happen,” but when we evaluate the underlying patterns, sleep disruption appears repeatedly. Insufficient sleep amplifies neural excitability, increases inflammation, and lowers your pain threshold. Even a single night of insomnia can trigger a migraine the next day. When this becomes consistent, the brain shifts into a chronic migraine cycle that becomes difficult to break without addressing the sleep problem itself.
When you don’t sleep well, deep neurological changes occur. The brain becomes overwhelmed, overstimulated, and unable to regulate pain signals effectively. During restorative sleep—particularly slow-wave sleep—the brain resets inflammatory markers, regulates neurotransmitters, and stabilizes pain pathways. When this stage of sleep is disrupted, these processes fall out of balance, making you more prone to migraines.
Sleep affects the brain in several ways that directly relate to migraines:
● Increased cortical excitability: The brain becomes overly reactive, making migraines much easier to trigger.
● Disrupted serotonin and dopamine levels: These neurotransmitters regulate pain, mood, and sleep; imbalance makes migraine pathways more active.
● Higher inflammation and stress hormones: Elevated cortisol and inflammatory cytokines create an environment where migraine pain can escalate rapidly.
● Poor glymphatic drainage: At night, the brain clears metabolic waste. When sleep is restricted, this system cannot function properly, increasing the likelihood of neurological irritation.
These mechanisms explain why someone may have multiple migraines a week without understanding that their sleep patterns are to blame. Fixing insomnia often reduces migraines dramatically because it restores stability to these essential brain systems.
There is a significant difference. Occasional insomnia—perhaps a restless night here and there—may cause a temporary headache the next day but usually does not drive chronic migraines. Chronic sleep deprivation, however, creates a cumulative effect that changes how the brain handles pain.
Insomnia becomes medically relevant when it starts occurring at least three times per week for three months or more. This pattern pushes the nervous system into a prolonged state of hyperactivation. Over time, the migraine threshold lowers, meaning even small triggers can set off intense headache episodes.
In short:
● Occasional insomnia may cause temporary symptoms.
● Chronic insomnia or long-term sleep deprivation can fundamentally alter pain pathways and contribute to chronic migraine diagnosis.
Understanding the distinction helps determine when lifestyle changes may be helpful—and when it’s time to seek professional sleep evaluation.
A sleep study becomes appropriate when insomnia is persistent, worsening, or clearly linked to your migraine pattern. Many patients reach us after years of treating migraines with medications, dietary changes, and lifestyle modifications, only to discover that an undiagnosed sleep disorder was the missing link.
You should consider a sleep study if:
● You regularly wake up with headaches or migraines.
● You struggle to fall asleep or stay asleep more than a few nights per week.
● You feel unrefreshed despite “sleeping enough hours.”
● You snore, gasp, or experience pauses in breathing during sleep.
● You grind your teeth or have TMJ-related pain associated with migraine episodes.
● Your migraines remain uncontrolled despite treatment.
● You notice an increase in migraines following poor sleep.
A sleep study (polysomnography) measures brain activity, breathing, muscle movement, oxygen levels, and sleep stages. This allows our specialists to determine whether insomnia, sleep apnea, upper-airway resistance syndrome, bruxism, or fragmented sleep architecture is contributing to your migraine condition.
For many patients, identifying and treating the sleep disorder reduces migraine frequency more effectively than years of medication cycles.
At Koala Center for Sleep & TMJ Disorders, we specialize in diagnosing and treating the sleep-related causes behind chronic migraines. Instead of focusing solely on pain relief, we evaluate the neurological and airway factors that disrupt sleep and amplify migraine activity.
Your personalized plan may include:
● Improving sleep architecture through behavioral or medical therapies
● Treating sleep apnea, bruxism, or TMJ disorders that worsen migraine patterns
● Stabilizing circadian rhythms to support consistent restorative sleep
● Reducing nighttime sympathetic activation so the brain can fully rest
● Implementing migraine-specific sleep strategies tailored to your physiology
Many of our patients experience fewer migraines, less intensity, and improved daily functioning once their sleep is restored—because their brain is finally getting the recovery it needs.
If your migraines are controlling your life, your sleep may be the key to breaking the cycle.
Can treating insomnia really reduce migraines?
Yes—improving sleep can significantly lower migraine frequency and severity.
Do migraines cause insomnia, or does insomnia cause migraines?
Both can occur, but insomnia is a major, often overlooked trigger.
Will fixing my sleep schedule alone stop migraines?
It helps, but many patients need deeper evaluation for hidden sleep disorders.

Additional Services You May Need
▸ KoalaKIDZzz®
▸ Sleep Apnea
▸ Snoring
▸ TMJ Disorder
▸ Fatigue
▸ Sleep Disorders
▸ Weight Loss
▸ CPAP Alternative
▸ Oral Appliances