What Is the Most Effective Way to Treat Hypnagogic Hallucinations in El Paso, TX?
Hypnagogic hallucinations (HH) are usually a sign of sleep disruption, not a standalone illness. To find the most effective treatment, Our providers at Koala Center For Sleep & TMJ Disorders in El Paso, TX, focus on accurate diagnosis. We use specialized testing to determine if your HH is an isolated event (often treatable through strict sleep hygiene) or a symptom of a primary sleep disorder like narcolepsy or severe sleep deprivation, which require targeted medical intervention. For more information, please contact us today or request an appointment online. We have convenient locations in Bloomington IL, Peoria/Dunlap IL, Mishawaka IN, El Paso TX, and Wausau WI.
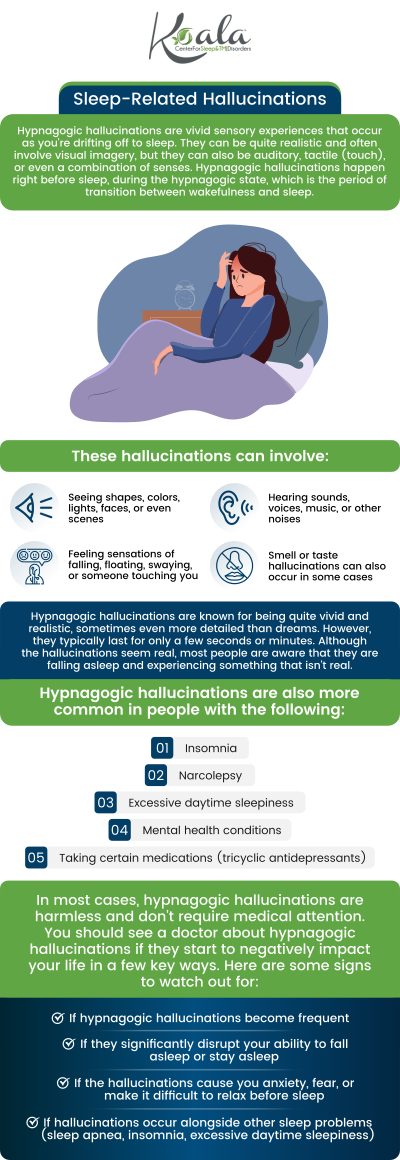
Table of Contents:
Is it just an isolated hypnagogic hallucination, or could it be a symptom of an underlying condition like narcolepsy or sleep apnea?
What is the process for differentiating HH from other sleep-related behaviors or psychiatric issues?
Is the frequency or intensity of HH episodes correlated with overall sleep debt?
What is the best way to cope with an HH episode while it is happening?
El Paso’s Specialist: Expert Treatment for Hypnagogic Hallucinations at Koala Center
Quick FAQ
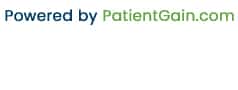
The most effective way to treat hypnagogic hallucinations (HH) begins with accurately identifying what is causing them—whether they are harmless, isolated sensory events or symptoms tied to a deeper sleep or neurological condition. At the Koala Center for Sleep & TMJ Disorders in El Paso, HH is evaluated through a medically structured approach that considers your sleep patterns, your airway, your psychological health, and the presence of other sleep-wake symptoms.
Because hypnagogic hallucinations occur while falling asleep, they can be frightening, confusing, or disruptive, especially when paired with sleep paralysis. Treatment relies on first understanding whether your episodes are benign or linked to disorders such as narcolepsy, REM-related disturbances, chronic sleep deprivation, or untreated obstructive sleep apnea (OSA). Here’s how our El Paso sleep specialists guide patients through the process of diagnosis and long-term management.
Many people experience an occasional hypnagogic hallucination, especially during periods of high stress, irregular sleep schedules, or significant sleep debt. When these episodes happen once in a while, they are often a normal response to transitions in the sleep-wake cycle. However, frequent or intense HH episodes may indicate something more.
A sleep specialist evaluates:
● Whether your hallucinations occur alone or are accompanied by sleep paralysis.
● If you have excessive daytime sleepiness—a hallmark sign of narcolepsy.
● Whether symptoms suggest airway obstruction, such as loud snoring, gasping, or choking during sleep.
● Sudden “sleep attacks” or abrupt muscle weakness, which may indicate narcolepsy with cataplexy.
When HH occurs alongside disrupted breathing, chronic fatigue, or fragmented sleep, it may signal undiagnosed sleep apnea. If it occurs with abnormal REM-related transitions, narcolepsy becomes more likely. Proper diagnosis prevents mislabeling the hallucinations as purely psychological or “stress-related” when they may be neurologically driven.
Hypnagogic hallucinations can look similar to nightmares, REM sleep behavior disorder, night terrors, or even certain psychiatric conditions, which is why not every hallucination should be interpreted the same way. At the Koala Center For Sleep & TMJ Disorders, the diagnostic process is structured, evidence-based, and focused on distinguishing HH from conditions that mimic it.
A sleep specialist typically conducts:
1. Comprehensive Sleep and Medical Evaluation: This includes reviewing medication history, psychiatric history, and lifestyle habits that may contribute to hallucination frequency.
2. Differentiation From Psychotic Disorders: HH occurs during transitions between wakefulness and sleep. Psychiatric hallucinations occur during full wakefulness and often have different thought-pattern characteristics. This timing distinction is crucial.
3. Polysomnography or MSLT (Multiple Sleep Latency Test) When Needed: These tests evaluate REM-sleep timing, airway issues, arousal patterns, and the speed at which you fall asleep—data essential for diagnosing narcolepsy or sleep apnea.
4. Assessment of Co-Occurring Sleep Disturbances: Conditions such as insomnia, circadian-rhythm dysregulation, or parasomnias can amplify HH episodes and must be addressed to achieve long-term improvement.
This methodical approach ensures HH is not misdiagnosed or oversimplified and leads to targeted treatment.
Yes, sleep debt can dramatically affect how often hypnagogic hallucinations occur. When the brain is forced into REM-like transitions too quickly—often due to chronic sleep deprivation—it may “bleed” dream-like imagery into moments when you are not yet fully asleep. This makes hallucinations more vivid, intrusive, and frightening.
A sleep specialist will review your sleep duration, consistency, and lifestyle factors that may contribute to sleep loss. In many cases, regulating sleep and restoring a healthy circadian rhythm reduces episode frequency significantly. However, if normalizing sleep does not improve symptoms, deeper neurological or REM-sleep disorders may be present.
Coping strategies are highly individualized, but several techniques help reduce fear and regain control during an episode:
● Remind yourself the event is temporary: HH episodes typically last seconds to a few minutes.
● Focus on small voluntary movements: Moving a finger or toe helps break lingering sleep paralysis and interrupts hallucination intensity.
● Use grounding techniques: Directing your mind to the texture of your sheets, the sound of a fan, or your breathing pattern helps pull the brain out of REM-like intrusions.
● Improve the sleep environment: A cool, dark, predictable sleep setting reduces nighttime confusion and rapid sleep-stage transitions.
Your clinician may also review light therapy, cognitive-behavioral sleep interventions, or structured relaxation strategies if anxiety worsens symptoms.
At the Koala Center for Sleep & TMJ Disorders, treatment for hypnagogic hallucinations is grounded in understanding the full picture—your sleep stages, airway function, breathing patterns, neurological markers, and lifestyle demands.
Our approach includes:
● Precision diagnostics with sleep studies when necessary
● Evaluation for narcolepsy, REM dysregulation, and sleep apnea
● Behavioral and environmental modifications
● Treatment of coexisting sleep disorders
● Ongoing monitoring to prevent recurrence
By addressing both the symptoms and their root causes, patients regain confidence and feel safe in their sleep transitions again.
Are hypnagogic hallucinations dangerous?
Not usually, but frequent episodes may indicate a deeper sleep disorder.
Can children experience hypnagogic hallucinations?
Yes, though they are less common; evaluation is recommended if episodes are repetitive or distressing.
Will treatment work if my HH is stress-related?
Yes—sleep stabilization, stress reduction, and lifestyle adjustments often reduce or eliminate episodes.
Check Out Our 5 Star Reviews


Additional Services You May Need
▸ KoalaKIDZzz®
▸ Sleep Apnea
▸ Snoring
▸ TMJ Disorder
▸ Fatigue
▸ Sleep Disorders
▸ Weight Loss
▸ CPAP Alternative
▸ Oral Appliances