Is My Headache Coming From a Migraine or My Jaw? How to Tell When TMJ Is the Real Cause
Many chronic headaches are misdiagnosed as migraines when the actual source is a misaligned bite or TMJ dysfunction. At Koala® Center For Sleep & TMJ Disorders, our specialists use a comprehensive neuromuscular evaluation to determine if your pain is triggered by jaw tension rather than neurological factors. For more information, please contact us today or request an appointment online. We have convenient locations in Bloomington IL, Peoria/Dunlap IL, El Paso TX, and Wausau WI.
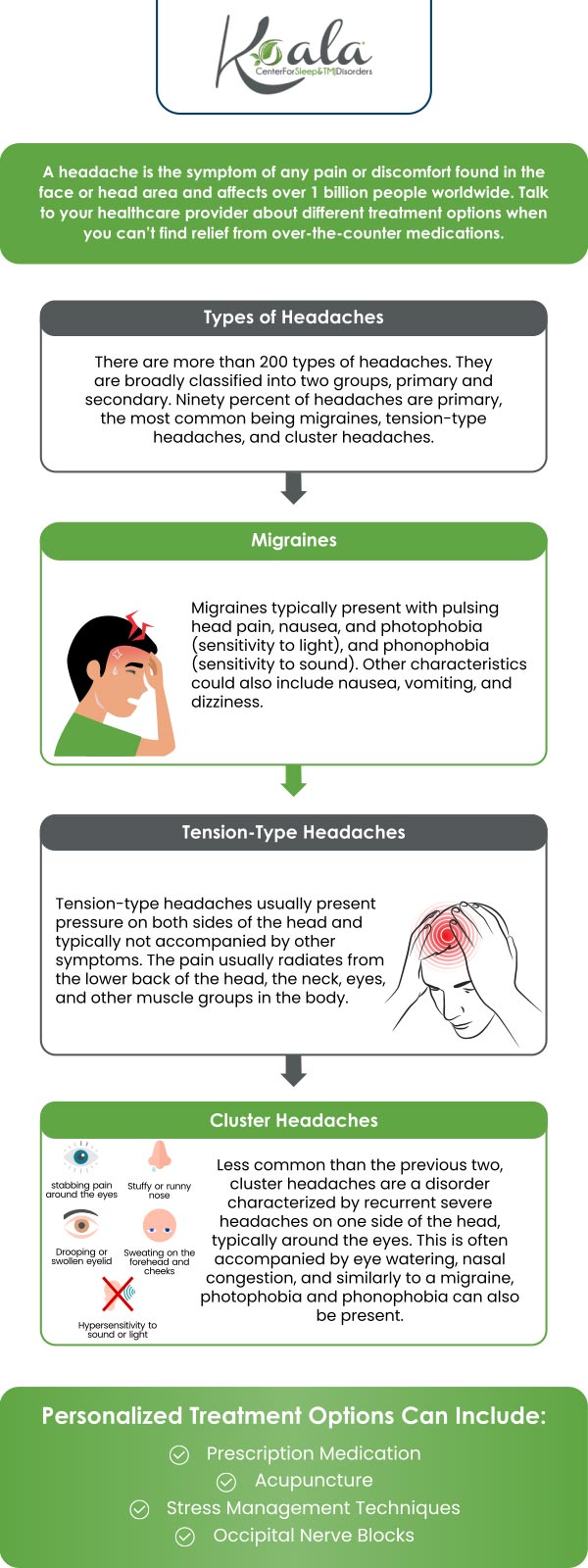
Table of Contents:
How can I tell if my headache is caused by TMJ disorder or a migraine?
What are the common symptoms of TMJ-related headaches?
What are the warning signs that a migraine is not related to jaw issues?
Can jaw clenching or teeth grinding trigger migraines?
A Personalized Perspective: Why TMJ Is Often Missed in Chronic Headache Patients
Why Correct Diagnosis Matters for Long-Term Relief
Frequently Asked Questions
Many patients struggle for years with recurring headaches, assuming they are migraines, only to discover later that the source is actually the jaw. Temporomandibular joint (TMJ) disorders and migraines can produce overlapping symptoms, which makes distinguishing between them challenging without proper evaluation. Understanding the warning signs can help you identify whether your headaches are neurologic in origin or driven by jaw dysfunction—and guide you toward the right treatment.
The most reliable way to differentiate TMJ-related headaches from migraines is to look at where the pain starts and what activities make it worse. TMJ headaches often originate near the jaw joint, just in front of the ears, and may radiate to the temples, cheeks, or forehead. They are frequently linked to jaw movement, such as chewing, yawning, talking for long periods, or waking up in the morning.
Migraines, by contrast, are neurological events. They often begin as a throbbing or pulsating pain on one side of the head and may intensify with light, sound, or physical activity. Migraines are less likely to worsen with jaw motion and more likely to be associated with sensory symptoms like visual disturbances or nausea.
Another important distinction is timing. TMJ-related headaches commonly coincide with jaw tension, stress, or sleep-related habits like clenching or grinding. Migraines may follow hormonal changes, dietary triggers, weather shifts, or sleep pattern disruptions that are unrelated to jaw mechanics.
TMJ-related headaches rarely occur in isolation. They are usually part of a broader pattern of jaw and facial symptoms that point to dysfunction in the temporomandibular joint and surrounding muscles.
Patients with TMJ headaches often report jaw stiffness or soreness, clicking or popping sounds when opening or closing the mouth, and difficulty opening the jaw fully. Pain may feel dull, achy, or pressure-like rather than throbbing. It often affects both sides of the head, especially the temples, and may extend into the ears, neck, or shoulders.
Morning headaches are another red flag for TMJ involvement. These often result from nighttime teeth grinding or clenching, which overloads the jaw muscles during sleep. Unlike migraines, TMJ headaches may improve temporarily with heat, gentle massage, or jaw rest.
Certain symptoms strongly suggest that a headache is neurologic rather than jaw-related. Migraines are commonly accompanied by nausea, vomiting, light sensitivity, sound sensitivity, or visual disturbances such as flashing lights or blind spots. These features are not typical of TMJ disorders.
Migraines also tend to follow predictable patterns or triggers that have little to do with jaw activity. Hormonal fluctuations, specific foods, dehydration, and changes in sleep cycles are classic migraine triggers. If your headache pain continues regardless of jaw position or movement, TMJ is less likely to be the primary cause.
Additionally, migraines often respond to migraine-specific medications, while TMJ headaches typically do not. If jaw-focused treatments like bite guards, physical therapy, or muscle relaxation provide relief, that points toward TMJ involvement rather than migraine pathology.
Jaw clenching and teeth grinding do not directly cause migraines, but they can act as powerful triggers in individuals who are already prone to them. Chronic clenching places sustained tension on the jaw, temples, and neck muscles, which can irritate surrounding nerves and increase overall head pain sensitivity.
In some patients, this muscular overload lowers the threshold for migraine attacks. The result is a headache that feels like a migraine but is being perpetuated—or intensified—by jaw dysfunction. This overlap is one reason misdiagnosis is common and why treating only the migraine symptoms may provide incomplete relief.
Addressing clenching or grinding through oral appliances, stress management, and jaw-focused therapy can significantly reduce headache frequency, even in patients with a history of migraines.
TMJ disorders are frequently overlooked because their symptoms mimic more familiar headache diagnoses. Many patients are treated for migraines for years without anyone examining how their jaw functions, how their teeth come together, or whether sleep-related grinding is present.
A comprehensive headache evaluation should include an assessment of jaw movement, muscle tenderness, bite alignment, and sleep habits. When TMJ dysfunction is identified and treated appropriately, patients often experience meaningful reductions in headache frequency, severity, and reliance on medication.
This integrated approach is especially important for patients whose headaches are resistant to standard migraine therapies or who notice pain worsening with chewing, talking, or stress.
Treating TMJ-related headaches as migraines can lead to unnecessary medication use without addressing the root cause. Conversely, assuming all headaches are jaw-related can delay proper neurologic care. Accurate diagnosis allows for targeted treatment, which may include oral appliances, physical therapy, behavioral strategies, or coordinated care between dental and medical providers.
When the jaw and nervous system are both considered, outcomes are often significantly better than treating either in isolation.
Can TMJ headaches feel exactly like migraines?
Yes, TMJ headaches can closely mimic migraines, especially when pain radiates to the temples or forehead.
Do migraines always cause nausea or visual symptoms?
No, but their presence strongly suggests a neurologic cause rather than TMJ dysfunction.
Should I see a dentist or a neurologist for chronic headaches?
Many patients benefit from evaluation by both, especially when jaw symptoms and headaches overlap.

Additional Services You May Need
▸ KoalaKIDZzz®
▸ Sleep Apnea
▸ Snoring
▸ TMJ Disorder
▸ Fatigue
▸ Sleep Disorders
▸ Weight Loss
▸ CPAP Alternative
▸ Oral Appliances